Volume 5, Issue 2 (2024)
J Clinic Care Skill 2024, 5(2): 103-110 |
Back to browse issues page
Article Type:
Subject:
Ethics code: IR.AJUMS.REC.1397.352
History
Received: 2024/02/6 | Accepted: 2024/06/11 | Published: 2024/06/27
Received: 2024/02/6 | Accepted: 2024/06/11 | Published: 2024/06/27
How to cite this article
Mashayekhi S, Abbaspoor Z, Cheraghian B, Javadnoori M. Men's Health Status in Pre-Pregnancy Care in Couples in Ahvaz Health Centers, Iran. J Clinic Care Skill 2024; 5 (2) :103-110
URL: http://jccs.yums.ac.ir/article-1-240-en.html
URL: http://jccs.yums.ac.ir/article-1-240-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Midwifery, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2- “Reproductive Health Promotion Research Center” and “Department of Midwifery, School of Nursing and Midwifery”, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
3- Department of Biostatistics and Epidemiology, School of Public Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2- “Reproductive Health Promotion Research Center” and “Department of Midwifery, School of Nursing and Midwifery”, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
3- Department of Biostatistics and Epidemiology, School of Public Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Full-Text (HTML) (1667 Views)
Introduction
Parents’ health before pregnancy is a crucial factor influencing pregnancy outcomes [1, 2]. Pre-pregnancy health promotion serves as a preventive strategy involving enhancing the health of couples to prepare for a natural pregnancy, maintain fertility, and identify and prevent risk factors [2]. Pre-pregnancy care involves implementing biomedical, behavioral, and social health interventions for couples before conception, with the goal of enhancing health and mitigating individual and environmental risk factors that contribute to adverse maternal and fetal outcomes [3]. The World Health Organization (WHO) has introduced pre-pregnancy care as a global action plan to reduce non-communicable diseases from 2013 to 2020 [4].
While the need for pre-pregnancy care for women is well-understood, with various comprehensive methods and measures in place [4, 5], equivalent measures for men are currently not widely and clearly defined [6]. Encouraging men to enhance their health behaviors before pregnancy and providing motivating information is crucial in enhancing pregnancy outcomes [7]. Men play a significant role in reproductive activities and should actively contribute to promoting sexual and reproductive health [1, 8]. Men may not fully grasp the impact of their health during pre-pregnancy on the quality of pregnancy outcomes [9]; therefore, it is essential to address their health alongside that of mothers in pre-pregnancy care.
Providing pre-pregnancy care for men offers numerous advantages. The primary benefit is enhancing the genetic and biological contribution of men to conception. Sperm can be compromised in various ways, including due to tobacco, alcohol, drug use, caffeine, poor diet, radiotherapy, chemotherapy, and testicular overheating. Conditions like diabetes, varicocele, and epididymitis are also linked to reduced sperm function. These impairments often lead to infertility, decreased fertility, or miscarriages. Furthermore, even if a pregnancy occurs and progresses, it can contribute to birth defects or childhood cancers in the offspring [10]. A recent review study indicated a lack of knowledge among men regarding pre-pregnancy health [11]. Another significant advantage of pre-pregnancy care for men is enhancing their readiness and comprehension of fatherhood. Men need to attain the cognitive and social maturity necessary to be effective parents, a process that can begin with pre-pregnancy care [12]. Ethically, fathers bear the responsibility to modify their behavior and mitigate controllable risk factors to enhance pregnancy outcomes, as many of the risk factors associated with men are modifiable and can reduce the severity of complications and harm to the mother or fetus [7, 13].
In recent years, attention has shifted towards pre-pregnancy care for men, leading to studies in this area. A study in the US revealed that half of men have limited knowledge about preconception health, with women being more acquainted with pre-pregnancy care than men [14]. Another study indicated that 60% of men aged 15 to 44 in the US require prenatal care, yet only a small percentage had undergone STD/HIV testing or counseling [8]. A study in Hungary reported that men receiving pre-pregnancy care are linked to a notable decrease in adverse pregnancy outcomes [15].
In studies conducted in Iran regarding pre-pregnancy care, the focus on men has primarily revolved around their involvement and support in receiving pre-pregnancy care for women [16, 17], rather than exploring men’s own health, considering their significant 50% biological contribution to conception health. The current study aimed to assess the health status of men concerning pre-pregnancy care among couples registered at healthcare centers in Ahvaz.
Instrument and methods
Study design
The present descriptive cross-sectional epidemiological study was carried out at designated health centers in Ahvaz City, Iran in 2019 and 2020.
Participants and sampling
The research population comprised married men whose wives were attending Ahvaz health centers for pre-pregnancy care or care during the first trimester of pregnancy. The sample size was determined to be 384 individuals by referencing a pertinent study [8], considering a 5% type I error and 80% test power using the following formula:
N=Z21-α/2 p(1-p)/d2
Where z21-α/2 was equal to 1.96, p was equal to 0.5, and d was equal to 0.05.
Sampling was conducted using a multi-stage method. Initially, three centers were chosen from the list of health centers in Ahvaz city, representing three distinct economic, social, and prosperous regions to facilitate participant access (one center from each region). Within each center, convenience sampling was carried out among eligible couples visiting the health centers for pre-pregnancy care, first-trimester pregnancy care, or child care, and with the intention of conceiving within the next six months. Inclusion criteria comprised married men intending to conceive within the next six months or whose partners were in the first trimester of pregnancy, possessing at least basic literacy skills in one spouse (to enable questionnaire reading), and being 18 years or older. Exclusion criteria encompassed known infertility or ongoing unplanned pregnancies.
Data collection tools and methods
A questionnaire was developed to gather data concerning the health status of men in pre-pregnancy care. Initially, through extensive research in the realm of male reproductive health and pre-pregnancy care for men, relevant variables were identified and structured into a questionnaire format using credible sources and current articles. Subsequently, to ascertain content validity, the questionnaire was reviewed by ten faculty members holding a Ph.D. in reproductive health or nursing. The final questionnaire was refined based on expert feedback and encompassed sections on demographic details, general health status, fertility, and medical history, spouse’s history of abortion or stillbirth, children’s abnormalities or diseases, substance abuse, medication usage, exposure to risk factors, and family history of genetic abnormalities.
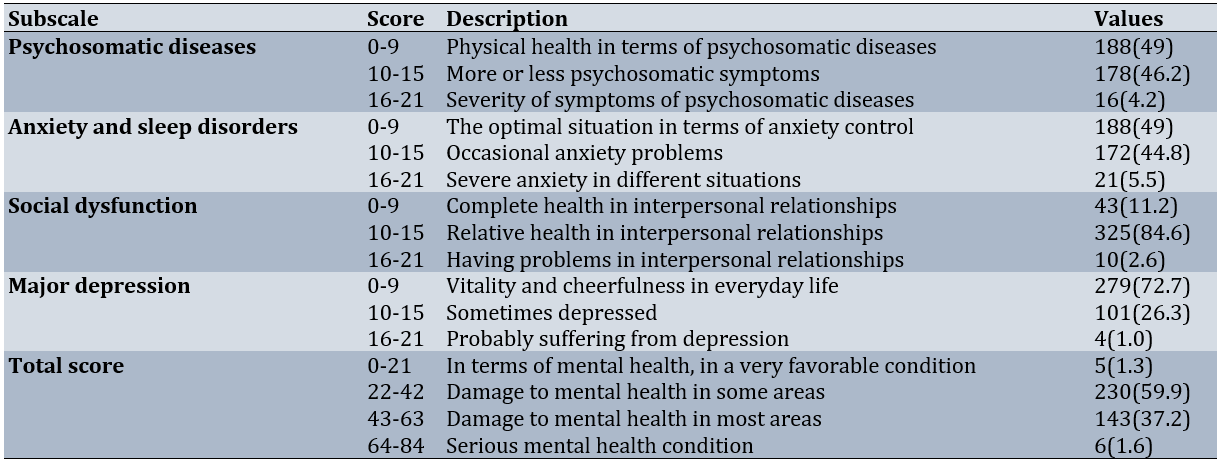
To assess men’s mental health, Goldberg and Hillier’s General Health Questionnaire (GHQ-28) was utilized. This questionnaire examines instances of psychological distress and comprises four subscales: physical symptoms, symptoms of anxiety and sleep disorders, social dysfunction, and severe depression. The total score ranges from 0 to 21, indicating very favorable mental health; 22 to 42 suggests a mental health concern in some areas; 43 to 63 indicates a mental health concern in many instances, while 64 to 84 signifies a severe mental health condition [18]. The questionnaire has been standardized in Iran [19] and has demonstrated good reliability [20].
Mothers attending the selected health centers for pre-pregnancy care or first-trimester pregnancy care were requested to encourage their husbands to visit the center if they wished to participate in the study. The research objectives were elucidated to the participants. Upon obtaining written informed consent, the men’s health status was assessed through questionnaires and tests to evaluate blood sugar and lipids, as well as by measuring height and weight to calculate BMI and blood pressure. Individuals were weighed in light clothing without shoes using a standard scale with a precision of 1kg, while their height without shoes was measured with a standing caliper accurate to 1cm.
The scale’s accuracy was verified using a standard weight of 500g. Blood pressure was measured using a dial sphygmomanometer. To minimize individual error, all measurements were conducted by a single individual (the first author). Body mass index (BMI) was computed by dividing weight (kg) by the square of height (m), and participants were categorized into four groups based on BMI: underweight <18.5, normal 18.5-24.9, overweight 25-29.9, and obese ≥30kg/m2. Sampling was carried out from November 22, 2019, to February 14, 2020, until a sufficient number of samples were obtained.
Data analysis
Data analysis was performed using SPSS 22 software, employing descriptive statistical methods such as frequency distribution tables, mean, and standard deviation. The relationship between qualitative variables was assessed using the chi-square test, with a significance level set at less than 0.05.
Findings
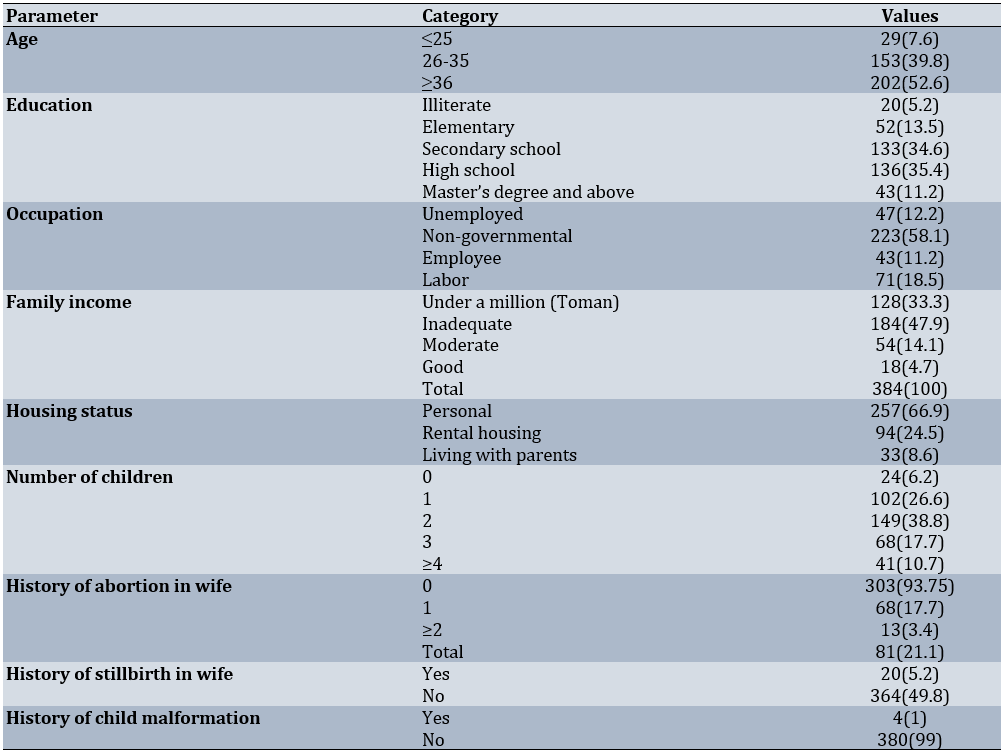
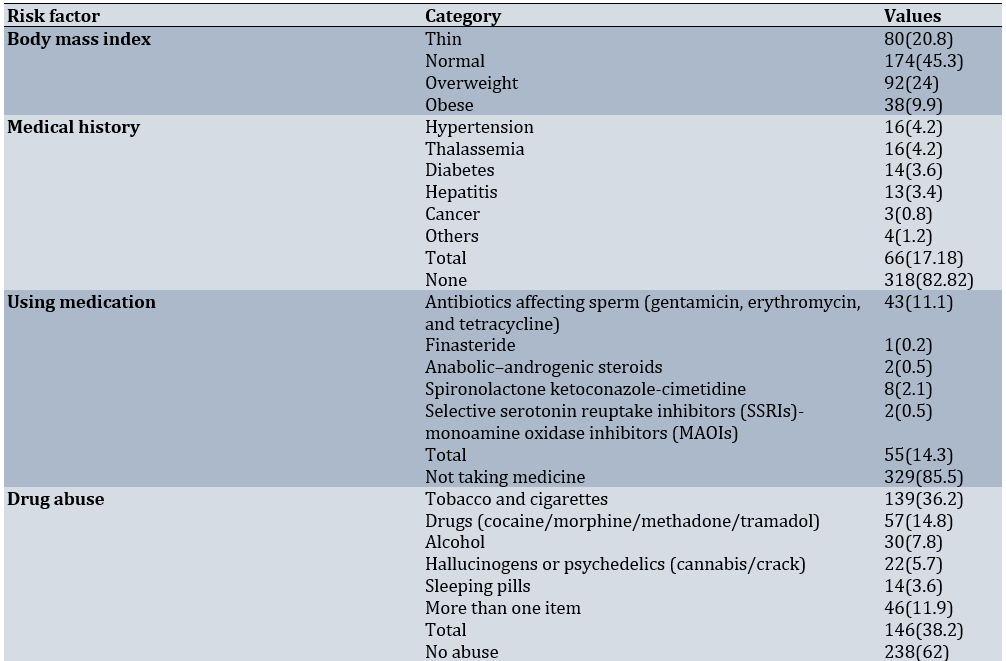
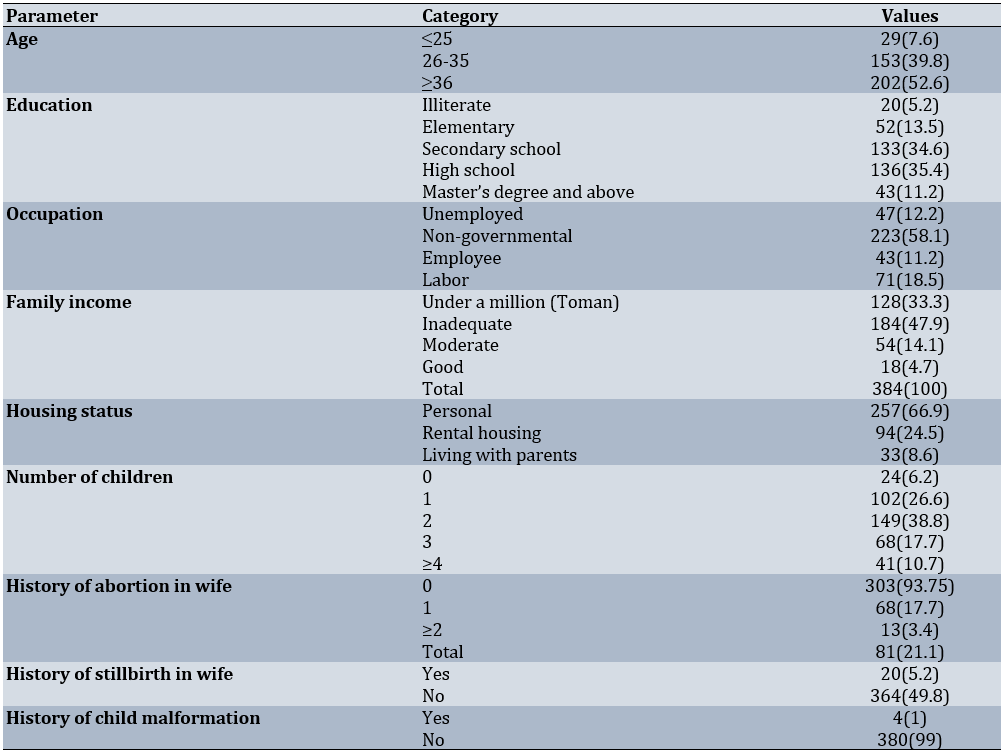
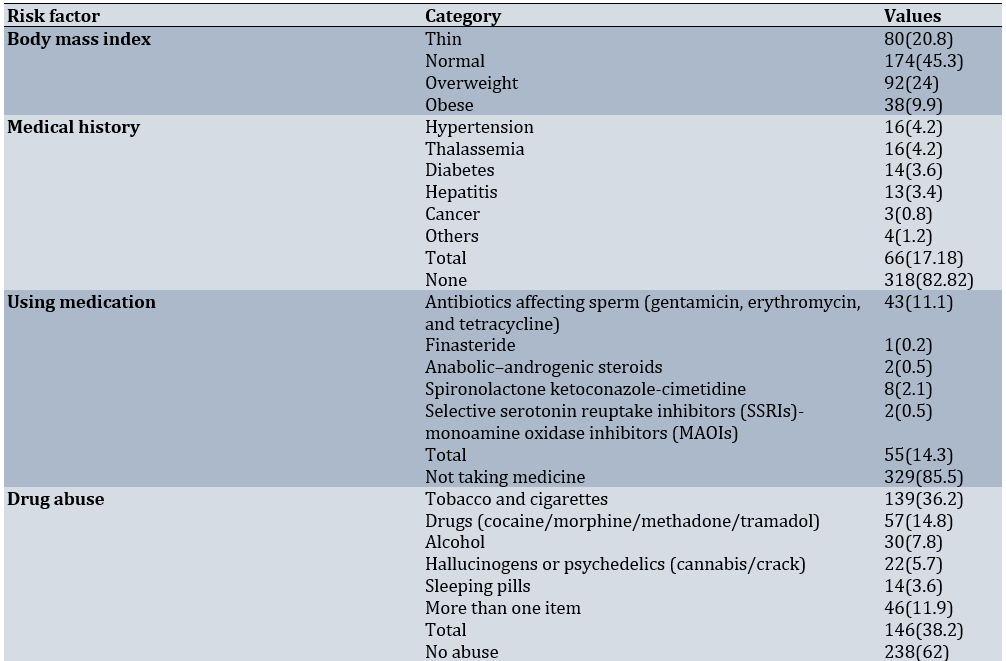
A total of 384 subjected were included in the study. The average age of the men was approximately 35 years, ranging from 22 to 63 years, with the majority falling between 30 and 40 years old (Table 1). In terms of BMI, 33.9% of the men were classified as overweight or obese. Approximately 17% of the men had at least one condition impacting fertility or fetal health, with prevalent diseases including high blood pressure, thalassemia, diabetes, and hepatitis. Moreover, around 14% of the men had taken medications known to have adverse effects on reproductive or fetal health, and about 38% had a history of drug abuse.
Table 1. Frequency of demographic and fertility characteristics of men participating in the research (n=384)
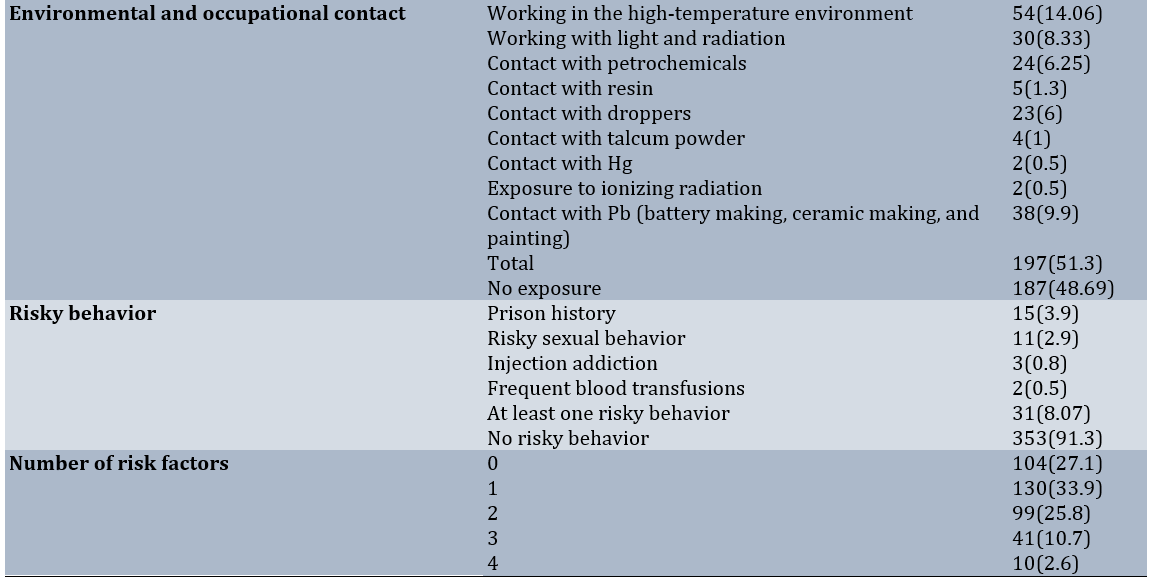
About half of the men had been exposed to at least one environmental or occupational pollutant, while approximately 10% engaged in risky behaviors (Table 2).
Table 2. Distribution of absolute and relative frequency of health indicators and risk factors before trying to get pregnant in men participating in the research (n=384)
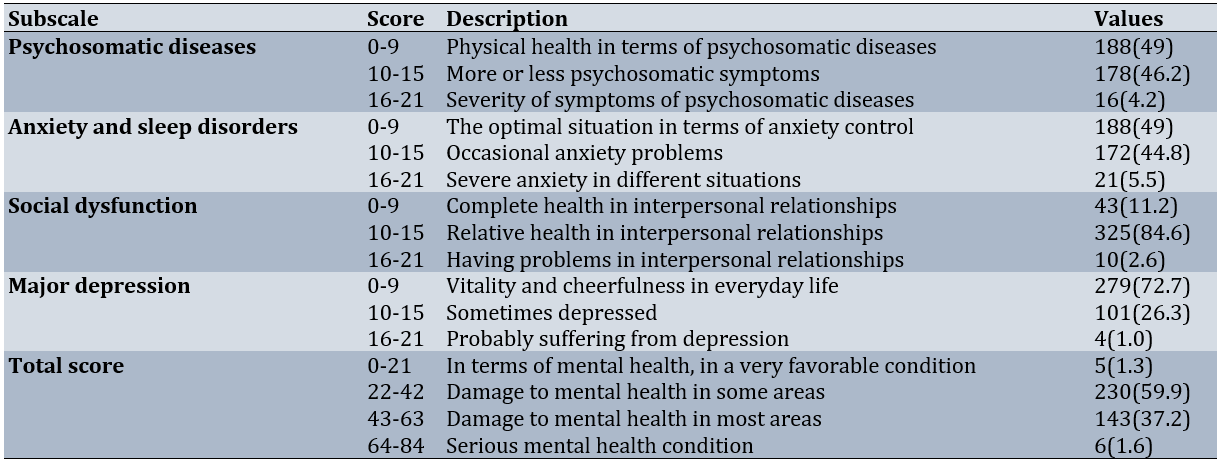
Regarding mental health, approximately 50% of men exhibited psychosomatic conditions, and an equal percentage displayed symptoms of anxiety and sleep disorders. Notably, 37.2% experienced significant mental health issues (Table 3).
Table 3. Mental health status of men prior to attempting conception (n=384)
Blood pressure and biochemical indices of men are also shown in Table 4.
Table 4. Frequency of blood pressure status and biochemical factors in men (n=384)

The history of drug abuse did not show a significant correlation with age or economic status (p>0.05), but it was notably associated with educational attainment (p<0.001). A majority of men with a history of drug abuse had completed middle school, whereas those without such a history had attained a diploma. Results from the Chi-square test indicated that a history of abortion or stillbirth in the wife did not exhibit statistically significant relationships with medical history (p=0.81), abnormal BMI (p=0.056), drug use (p=0.09), drug abuse (p=0.7), or exposure to pollutants or occupational hazards (p=0.2; Table 5).
Table 5. Absolute and relative frequency of history of abortion/stillbirth by risk factors in men

Discussion
The current study aimed to evaluate the health status of men receiving pre-pregnancy care within couples under the purview of health centers in Ahvaz, Iran. This research marks the initial investigation into the health status of men undergoing pre-pregnancy care in Iran. Findings revealed that a notable proportion of men attempted conception despite having at least one risk factor jeopardizing the health of conception or the well-being of the fetus/newborn.
The age range of the men in the study spanned from 22 to 63 years. Given the rising age of marriage and a notable decline in fertility rates in Iran, the impact of advancing paternal age on pregnancy outcomes and fetal health has been under scrutiny. While numerous studies have explored the correlation between advanced maternal age and adverse pregnancy outcomes, research on the influence of advanced paternal age on pregnancy outcomes remains limited. A recent review study linked advanced paternal age to a moderate uptick in the occurrence of genital, cardiovascular, and facial deformities, and chromosomal disorders [21]. In general, as age increases, testicular function and sperm parameters tend to diminish, leading to a rise in germline sperm mutations and genetic irregularities. Furthermore, the epigenetic effects of age on sperm should not be overlooked [22]. Notably, in a Hungarian study, approximately 6% of men seeking prenatal care were aged over 50 years [15]. It is crucial to educate couples on the risks associated with delaying parenthood until later years within the fertility window and to discourage prolonged birth spacing. This guidance should be integrated into pre-pregnancy and family planning counseling sessions for couples.
In the current study, 34% of men were classified as overweight or obese. Previous studies in Iran have indicated that the prevalence of obesity or overweight (BMI greater than 25kg/m2) among men is approximately 50% [23]. A study examining pre-pregnancy risk factors in Italy reported an obesity prevalence (BMI above 30) of around 8% [24]. However, in the mentioned study, data collection relied on an online questionnaire, potentially raising concerns about data accuracy. In contrast, BMI measurements in the present study were conducted by the researcher. In a study conducted in the US, the prevalence of obesity among men aged 15 to 44 seeking pre-pregnancy care was reported to be about 56% [8]. Numerous studies have highlighted the adverse impact of being overweight particularly obesity on male fertility [25-28]. Weight gain in men is associated with a decrease in serum testosterone concentration, which can negatively affect sperm concentration and quality [28, 29]. Given that obesity is recognized as a risk factor for fertility and pregnancy outcomes, approximately 10% of the men in the current study exhibited this risk factor. As weight management or loss is a time-intensive process, it is imperative to offer nutritional guidance to address weight concerns in men desiring to start a family with the same level of attention provided to women.
The analysis of biochemical factors, such as blood glucose and lipid profiles, revealed that approximately 4-9% of men had conceived while exhibiting abnormalities in these factors, and around 9% of men had high blood pressure. It is worth noting that while about 20% of the men studied had elevated or borderline blood pressure readings, only 4% of them reported a history of high blood pressure.
In the current study, a notable proportion of men exhibited unfavorable conditions in each of the mental health scales. Mental health was compromised in 37% of men across various domains. Despite the wealth of research on the influence of different facets of maternal mental health on pregnancy, childbirth, and newborns, a comprehensive search by the authors revealed limited studies on the impact of men’s mental health prior to pregnancy on fetal health and pregnancy outcomes. While several studies have explored men’s mental health during pregnancy, postpartum periods, and the transition to fatherhood, research specifically focusing on men’s mental health before pregnancy remains scarce [30].
Approximately 14% of the men were using a drug that could potentially have a negative impact on fertility or fetal health. In a study conducted by Crijns et al., around 35% of men have taken at least one medication before pregnancy [31]. A study in Italy, analyzing calls received by men at the teratology information service, revealed that approximately 1% of the yearly calls are from men. Among these calls, 76% pertain to drug exposure, 17% to exposure to anti-cancer treatments (chemotherapy and/or radiotherapy), 4% to contact with diagnostic radiation, 2% to substance abuse, and 1% to occupational exposure [32]. In a comprehensive cohort study in Norway investigating the link between paternal drug exposure before pregnancy and pregnancy outcomes such as preterm birth, perinatal death, growth restriction, and birth defects, researchers discovered that about a quarter of fathers have been exposed to at least one drug in the three months leading up to pregnancy. The rate was 1.3% for drugs necessitating special attention. Overall, the assessment of pregnancy outcomes in two groups of men do not reveal a significant difference in the occurrence of adverse pregnancy outcomes. However, in cases involving diazepam usage, the rate of perinatal death and growth restriction is notably higher in the group of users [33]. It is crucial to note that due to the duration of spermatogenesis, men should be equipped with adequate knowledge that occupational or environmental exposures, as well as drug usage, can be significant even for three months before attempting to conceive. It is essential to explore the potential effects of drugs on pregnancy outcomes and consult a healthcare provider to take necessary actions, such as considering postponing pregnancy, altering medication, or adjusting medication dosages.
In the current study, approximately 38% of men reported some form of substance abuse. A study conducted in the Netherlands revealed that paternal smoking before pregnancy is linked to an increased risk of anorectal abnormalities [34]. Another study indicated that 58% of men seeking pre-pregnancy care have consumed alcohol within the past year, with 21% engaging in sexually risky behavior [8]. Some studies have indicated that men do not alter their alcohol and marijuana consumption habits before pregnancy [35]. While extensive research has been carried out on maternal drug abuse during pregnancy [36], the impact of paternal substance abuse before pregnancy on pregnancy outcomes has received less attention.
Roughly half of the men in this study had occupational exposure to at least one pollutant, with the most common exposures being linked to working in high-temperature environments and contact with light and radiation. Research has shown that the serum concentration of certain pollutants in the blood of the father and/or mother before pregnancy is correlated with lower baby weight [37]. Some paternal occupational exposures have been linked to an increased risk of anorectal abnormalities [34]. A recent review study highlighted that individuals experiencing fertility parameter disruptions are more likely to be exposed to environmental and occupational risk factors [38]. One challenge in examining the effects of occupational exposures on sperm parameters and sperm DNA damage is the complexity of isolating the impact of each factor individually. In many instances, individuals are simultaneously exposed to multiple factors. For instance, professional drivers, in addition to facing the risk factor of prolonged sitting, may experience chemical exposure, noise, social stress, pressure on pelvic organs, and increased temperatures, all contributing to an elevated risk of spermatogenesis damage [39]. This complexity also applies to welders who encounter solvents, heavy metals, and noise in their work environments.
In a study conducted in Iran, it was revealed that men’s requirement for enhancing fatherly role skills rank as the third priority among their perceived needs (57%) and unmet needs (85%) in the realm of health services [40].
One of the major challenges in addressing men’s health before pregnancy is the comparative lack of research on pre-pregnancy care standards for men in contrast to those available for women [41]. Another significant hurdle is the limited awareness among health service providers regarding men’s pre-pregnancy health [42].
This study marks the first examination of men’s health before pregnancy in Iran, serving as a foundational piece for future research in this area, despite its limitations. One limitation is that the research sample comprised solely married men under the coverage of health centers, thus the findings may not be universally applicable to all men in Ahvaz. Additionally, the health status, including blood pressure and test results, of men whose wives were in the first trimester of pregnancy could differ from before pregnancy. Another consideration pertains to men’s comprehension of questions and the accuracy of their responses regarding exposure to pollutants and occupational hazards, which may introduce reliability issues. Moreover, the lack of extensive investigation into pre-pregnancy care standards for men poses challenges in defining investigation criteria and risk factors, thereby presenting significant hurdles for studies in this field.
The evaluation of men in preconception care can aid in identifying risk factors that impact male fertility, and reproductive health, and ultimately enhance pregnancy outcomes. By pinpointing these risk factors, educational initiatives can be implemented to raise men’s awareness. For couples planning to conceive, it is crucial for men to seek care, identify potential risk factors, and make necessary adjustments. Given that the effects of certain medications and pollutants can persist over an extended period, it is advisable to recommend couples undergo a check-up at least one year before attempting to conceive. While it appears that there is currently a lack of adequate services, capacity, and infrastructure in health centers to offer pre-pregnancy services to men on a broad scale, careful planning is essential to extend these services. The existing programs within the primary healthcare system, which already cater to men through initiatives like the middle-aged program or pre-pregnancy care program for women, serve as a suitable platform to address this crucial aspect of family health. Gynecologists, midwives, and other primary healthcare providers can play a pivotal role in encouraging men to seek preconception care. A significant factor in this process may be the insufficient awareness among healthcare providers themselves. In alignment with Iran’s population policies aimed at safeguarding the population, prioritizing the involvement of men is crucial. Given the research limitations, it is recommended that future studies focus on a population consisting solely of couples intending to conceive within the next six months
Conclusion
A significant number of men have tried to conceive while having at least one risk factor affecting the health of conception or the health of the fetus/newborn.
Acknowledgments: This article is derived from the midwifery master’s thesis of Somayeh Mashayekhi, registered at Ahvaz Jundishapur University of Medical Sciences. The authors express gratitude to the pregnant women who took part in the study, as well as to Ahvaz Jundishapur University of Medical Sciences for providing financial support for the research.
Conflicts of Interests: The authors declared no conflicts of interests.
Ethical Permissions: The study received approval from the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1397.352). To adhere to ethical standards, informed consent was acquired following a detailed explanation of the research objectives to the participants. Furthermore, the results were disclosed in accordance with confidentiality principles, ensuring anonymity by refraining from mentioning any names.
Authors’ Contribution: Mashayekhi S (First Author), Introduction Writer/Main Researcher/Discussion Writer (30%); Abbaspoor Z (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (15%); Cheraghian B (Third Author), Discussion Writer/Statistical Analyst (15%); Javadnoori M Introduction Writer/Methodologist/Main Researcher/Discussion Writer (40%)
Funding/Support: This study was supported by the Jundishapur University of Medical Sciences (Grant No.: RHPRC-9705).
Parents’ health before pregnancy is a crucial factor influencing pregnancy outcomes [1, 2]. Pre-pregnancy health promotion serves as a preventive strategy involving enhancing the health of couples to prepare for a natural pregnancy, maintain fertility, and identify and prevent risk factors [2]. Pre-pregnancy care involves implementing biomedical, behavioral, and social health interventions for couples before conception, with the goal of enhancing health and mitigating individual and environmental risk factors that contribute to adverse maternal and fetal outcomes [3]. The World Health Organization (WHO) has introduced pre-pregnancy care as a global action plan to reduce non-communicable diseases from 2013 to 2020 [4].
While the need for pre-pregnancy care for women is well-understood, with various comprehensive methods and measures in place [4, 5], equivalent measures for men are currently not widely and clearly defined [6]. Encouraging men to enhance their health behaviors before pregnancy and providing motivating information is crucial in enhancing pregnancy outcomes [7]. Men play a significant role in reproductive activities and should actively contribute to promoting sexual and reproductive health [1, 8]. Men may not fully grasp the impact of their health during pre-pregnancy on the quality of pregnancy outcomes [9]; therefore, it is essential to address their health alongside that of mothers in pre-pregnancy care.
Providing pre-pregnancy care for men offers numerous advantages. The primary benefit is enhancing the genetic and biological contribution of men to conception. Sperm can be compromised in various ways, including due to tobacco, alcohol, drug use, caffeine, poor diet, radiotherapy, chemotherapy, and testicular overheating. Conditions like diabetes, varicocele, and epididymitis are also linked to reduced sperm function. These impairments often lead to infertility, decreased fertility, or miscarriages. Furthermore, even if a pregnancy occurs and progresses, it can contribute to birth defects or childhood cancers in the offspring [10]. A recent review study indicated a lack of knowledge among men regarding pre-pregnancy health [11]. Another significant advantage of pre-pregnancy care for men is enhancing their readiness and comprehension of fatherhood. Men need to attain the cognitive and social maturity necessary to be effective parents, a process that can begin with pre-pregnancy care [12]. Ethically, fathers bear the responsibility to modify their behavior and mitigate controllable risk factors to enhance pregnancy outcomes, as many of the risk factors associated with men are modifiable and can reduce the severity of complications and harm to the mother or fetus [7, 13].
In recent years, attention has shifted towards pre-pregnancy care for men, leading to studies in this area. A study in the US revealed that half of men have limited knowledge about preconception health, with women being more acquainted with pre-pregnancy care than men [14]. Another study indicated that 60% of men aged 15 to 44 in the US require prenatal care, yet only a small percentage had undergone STD/HIV testing or counseling [8]. A study in Hungary reported that men receiving pre-pregnancy care are linked to a notable decrease in adverse pregnancy outcomes [15].
In studies conducted in Iran regarding pre-pregnancy care, the focus on men has primarily revolved around their involvement and support in receiving pre-pregnancy care for women [16, 17], rather than exploring men’s own health, considering their significant 50% biological contribution to conception health. The current study aimed to assess the health status of men concerning pre-pregnancy care among couples registered at healthcare centers in Ahvaz.
Instrument and methods
Study design
The present descriptive cross-sectional epidemiological study was carried out at designated health centers in Ahvaz City, Iran in 2019 and 2020.
Participants and sampling
The research population comprised married men whose wives were attending Ahvaz health centers for pre-pregnancy care or care during the first trimester of pregnancy. The sample size was determined to be 384 individuals by referencing a pertinent study [8], considering a 5% type I error and 80% test power using the following formula:
N=Z21-α/2 p(1-p)/d2
Where z21-α/2 was equal to 1.96, p was equal to 0.5, and d was equal to 0.05.
Sampling was conducted using a multi-stage method. Initially, three centers were chosen from the list of health centers in Ahvaz city, representing three distinct economic, social, and prosperous regions to facilitate participant access (one center from each region). Within each center, convenience sampling was carried out among eligible couples visiting the health centers for pre-pregnancy care, first-trimester pregnancy care, or child care, and with the intention of conceiving within the next six months. Inclusion criteria comprised married men intending to conceive within the next six months or whose partners were in the first trimester of pregnancy, possessing at least basic literacy skills in one spouse (to enable questionnaire reading), and being 18 years or older. Exclusion criteria encompassed known infertility or ongoing unplanned pregnancies.
Data collection tools and methods
A questionnaire was developed to gather data concerning the health status of men in pre-pregnancy care. Initially, through extensive research in the realm of male reproductive health and pre-pregnancy care for men, relevant variables were identified and structured into a questionnaire format using credible sources and current articles. Subsequently, to ascertain content validity, the questionnaire was reviewed by ten faculty members holding a Ph.D. in reproductive health or nursing. The final questionnaire was refined based on expert feedback and encompassed sections on demographic details, general health status, fertility, and medical history, spouse’s history of abortion or stillbirth, children’s abnormalities or diseases, substance abuse, medication usage, exposure to risk factors, and family history of genetic abnormalities.
To assess men’s mental health, Goldberg and Hillier’s General Health Questionnaire (GHQ-28) was utilized. This questionnaire examines instances of psychological distress and comprises four subscales: physical symptoms, symptoms of anxiety and sleep disorders, social dysfunction, and severe depression. The total score ranges from 0 to 21, indicating very favorable mental health; 22 to 42 suggests a mental health concern in some areas; 43 to 63 indicates a mental health concern in many instances, while 64 to 84 signifies a severe mental health condition [18]. The questionnaire has been standardized in Iran [19] and has demonstrated good reliability [20].
Mothers attending the selected health centers for pre-pregnancy care or first-trimester pregnancy care were requested to encourage their husbands to visit the center if they wished to participate in the study. The research objectives were elucidated to the participants. Upon obtaining written informed consent, the men’s health status was assessed through questionnaires and tests to evaluate blood sugar and lipids, as well as by measuring height and weight to calculate BMI and blood pressure. Individuals were weighed in light clothing without shoes using a standard scale with a precision of 1kg, while their height without shoes was measured with a standing caliper accurate to 1cm.
The scale’s accuracy was verified using a standard weight of 500g. Blood pressure was measured using a dial sphygmomanometer. To minimize individual error, all measurements were conducted by a single individual (the first author). Body mass index (BMI) was computed by dividing weight (kg) by the square of height (m), and participants were categorized into four groups based on BMI: underweight <18.5, normal 18.5-24.9, overweight 25-29.9, and obese ≥30kg/m2. Sampling was carried out from November 22, 2019, to February 14, 2020, until a sufficient number of samples were obtained.
Data analysis
Data analysis was performed using SPSS 22 software, employing descriptive statistical methods such as frequency distribution tables, mean, and standard deviation. The relationship between qualitative variables was assessed using the chi-square test, with a significance level set at less than 0.05.
Findings
A total of 384 subjected were included in the study. The average age of the men was approximately 35 years, ranging from 22 to 63 years, with the majority falling between 30 and 40 years old (Table 1). In terms of BMI, 33.9% of the men were classified as overweight or obese. Approximately 17% of the men had at least one condition impacting fertility or fetal health, with prevalent diseases including high blood pressure, thalassemia, diabetes, and hepatitis. Moreover, around 14% of the men had taken medications known to have adverse effects on reproductive or fetal health, and about 38% had a history of drug abuse.
Table 1. Frequency of demographic and fertility characteristics of men participating in the research (n=384)
About half of the men had been exposed to at least one environmental or occupational pollutant, while approximately 10% engaged in risky behaviors (Table 2).
Table 2. Distribution of absolute and relative frequency of health indicators and risk factors before trying to get pregnant in men participating in the research (n=384)
Regarding mental health, approximately 50% of men exhibited psychosomatic conditions, and an equal percentage displayed symptoms of anxiety and sleep disorders. Notably, 37.2% experienced significant mental health issues (Table 3).
Table 3. Mental health status of men prior to attempting conception (n=384)
Blood pressure and biochemical indices of men are also shown in Table 4.
Table 4. Frequency of blood pressure status and biochemical factors in men (n=384)

The history of drug abuse did not show a significant correlation with age or economic status (p>0.05), but it was notably associated with educational attainment (p<0.001). A majority of men with a history of drug abuse had completed middle school, whereas those without such a history had attained a diploma. Results from the Chi-square test indicated that a history of abortion or stillbirth in the wife did not exhibit statistically significant relationships with medical history (p=0.81), abnormal BMI (p=0.056), drug use (p=0.09), drug abuse (p=0.7), or exposure to pollutants or occupational hazards (p=0.2; Table 5).
Table 5. Absolute and relative frequency of history of abortion/stillbirth by risk factors in men

Discussion
The current study aimed to evaluate the health status of men receiving pre-pregnancy care within couples under the purview of health centers in Ahvaz, Iran. This research marks the initial investigation into the health status of men undergoing pre-pregnancy care in Iran. Findings revealed that a notable proportion of men attempted conception despite having at least one risk factor jeopardizing the health of conception or the well-being of the fetus/newborn.
The age range of the men in the study spanned from 22 to 63 years. Given the rising age of marriage and a notable decline in fertility rates in Iran, the impact of advancing paternal age on pregnancy outcomes and fetal health has been under scrutiny. While numerous studies have explored the correlation between advanced maternal age and adverse pregnancy outcomes, research on the influence of advanced paternal age on pregnancy outcomes remains limited. A recent review study linked advanced paternal age to a moderate uptick in the occurrence of genital, cardiovascular, and facial deformities, and chromosomal disorders [21]. In general, as age increases, testicular function and sperm parameters tend to diminish, leading to a rise in germline sperm mutations and genetic irregularities. Furthermore, the epigenetic effects of age on sperm should not be overlooked [22]. Notably, in a Hungarian study, approximately 6% of men seeking prenatal care were aged over 50 years [15]. It is crucial to educate couples on the risks associated with delaying parenthood until later years within the fertility window and to discourage prolonged birth spacing. This guidance should be integrated into pre-pregnancy and family planning counseling sessions for couples.
In the current study, 34% of men were classified as overweight or obese. Previous studies in Iran have indicated that the prevalence of obesity or overweight (BMI greater than 25kg/m2) among men is approximately 50% [23]. A study examining pre-pregnancy risk factors in Italy reported an obesity prevalence (BMI above 30) of around 8% [24]. However, in the mentioned study, data collection relied on an online questionnaire, potentially raising concerns about data accuracy. In contrast, BMI measurements in the present study were conducted by the researcher. In a study conducted in the US, the prevalence of obesity among men aged 15 to 44 seeking pre-pregnancy care was reported to be about 56% [8]. Numerous studies have highlighted the adverse impact of being overweight particularly obesity on male fertility [25-28]. Weight gain in men is associated with a decrease in serum testosterone concentration, which can negatively affect sperm concentration and quality [28, 29]. Given that obesity is recognized as a risk factor for fertility and pregnancy outcomes, approximately 10% of the men in the current study exhibited this risk factor. As weight management or loss is a time-intensive process, it is imperative to offer nutritional guidance to address weight concerns in men desiring to start a family with the same level of attention provided to women.
The analysis of biochemical factors, such as blood glucose and lipid profiles, revealed that approximately 4-9% of men had conceived while exhibiting abnormalities in these factors, and around 9% of men had high blood pressure. It is worth noting that while about 20% of the men studied had elevated or borderline blood pressure readings, only 4% of them reported a history of high blood pressure.
In the current study, a notable proportion of men exhibited unfavorable conditions in each of the mental health scales. Mental health was compromised in 37% of men across various domains. Despite the wealth of research on the influence of different facets of maternal mental health on pregnancy, childbirth, and newborns, a comprehensive search by the authors revealed limited studies on the impact of men’s mental health prior to pregnancy on fetal health and pregnancy outcomes. While several studies have explored men’s mental health during pregnancy, postpartum periods, and the transition to fatherhood, research specifically focusing on men’s mental health before pregnancy remains scarce [30].
Approximately 14% of the men were using a drug that could potentially have a negative impact on fertility or fetal health. In a study conducted by Crijns et al., around 35% of men have taken at least one medication before pregnancy [31]. A study in Italy, analyzing calls received by men at the teratology information service, revealed that approximately 1% of the yearly calls are from men. Among these calls, 76% pertain to drug exposure, 17% to exposure to anti-cancer treatments (chemotherapy and/or radiotherapy), 4% to contact with diagnostic radiation, 2% to substance abuse, and 1% to occupational exposure [32]. In a comprehensive cohort study in Norway investigating the link between paternal drug exposure before pregnancy and pregnancy outcomes such as preterm birth, perinatal death, growth restriction, and birth defects, researchers discovered that about a quarter of fathers have been exposed to at least one drug in the three months leading up to pregnancy. The rate was 1.3% for drugs necessitating special attention. Overall, the assessment of pregnancy outcomes in two groups of men do not reveal a significant difference in the occurrence of adverse pregnancy outcomes. However, in cases involving diazepam usage, the rate of perinatal death and growth restriction is notably higher in the group of users [33]. It is crucial to note that due to the duration of spermatogenesis, men should be equipped with adequate knowledge that occupational or environmental exposures, as well as drug usage, can be significant even for three months before attempting to conceive. It is essential to explore the potential effects of drugs on pregnancy outcomes and consult a healthcare provider to take necessary actions, such as considering postponing pregnancy, altering medication, or adjusting medication dosages.
In the current study, approximately 38% of men reported some form of substance abuse. A study conducted in the Netherlands revealed that paternal smoking before pregnancy is linked to an increased risk of anorectal abnormalities [34]. Another study indicated that 58% of men seeking pre-pregnancy care have consumed alcohol within the past year, with 21% engaging in sexually risky behavior [8]. Some studies have indicated that men do not alter their alcohol and marijuana consumption habits before pregnancy [35]. While extensive research has been carried out on maternal drug abuse during pregnancy [36], the impact of paternal substance abuse before pregnancy on pregnancy outcomes has received less attention.
Roughly half of the men in this study had occupational exposure to at least one pollutant, with the most common exposures being linked to working in high-temperature environments and contact with light and radiation. Research has shown that the serum concentration of certain pollutants in the blood of the father and/or mother before pregnancy is correlated with lower baby weight [37]. Some paternal occupational exposures have been linked to an increased risk of anorectal abnormalities [34]. A recent review study highlighted that individuals experiencing fertility parameter disruptions are more likely to be exposed to environmental and occupational risk factors [38]. One challenge in examining the effects of occupational exposures on sperm parameters and sperm DNA damage is the complexity of isolating the impact of each factor individually. In many instances, individuals are simultaneously exposed to multiple factors. For instance, professional drivers, in addition to facing the risk factor of prolonged sitting, may experience chemical exposure, noise, social stress, pressure on pelvic organs, and increased temperatures, all contributing to an elevated risk of spermatogenesis damage [39]. This complexity also applies to welders who encounter solvents, heavy metals, and noise in their work environments.
In a study conducted in Iran, it was revealed that men’s requirement for enhancing fatherly role skills rank as the third priority among their perceived needs (57%) and unmet needs (85%) in the realm of health services [40].
One of the major challenges in addressing men’s health before pregnancy is the comparative lack of research on pre-pregnancy care standards for men in contrast to those available for women [41]. Another significant hurdle is the limited awareness among health service providers regarding men’s pre-pregnancy health [42].
This study marks the first examination of men’s health before pregnancy in Iran, serving as a foundational piece for future research in this area, despite its limitations. One limitation is that the research sample comprised solely married men under the coverage of health centers, thus the findings may not be universally applicable to all men in Ahvaz. Additionally, the health status, including blood pressure and test results, of men whose wives were in the first trimester of pregnancy could differ from before pregnancy. Another consideration pertains to men’s comprehension of questions and the accuracy of their responses regarding exposure to pollutants and occupational hazards, which may introduce reliability issues. Moreover, the lack of extensive investigation into pre-pregnancy care standards for men poses challenges in defining investigation criteria and risk factors, thereby presenting significant hurdles for studies in this field.
The evaluation of men in preconception care can aid in identifying risk factors that impact male fertility, and reproductive health, and ultimately enhance pregnancy outcomes. By pinpointing these risk factors, educational initiatives can be implemented to raise men’s awareness. For couples planning to conceive, it is crucial for men to seek care, identify potential risk factors, and make necessary adjustments. Given that the effects of certain medications and pollutants can persist over an extended period, it is advisable to recommend couples undergo a check-up at least one year before attempting to conceive. While it appears that there is currently a lack of adequate services, capacity, and infrastructure in health centers to offer pre-pregnancy services to men on a broad scale, careful planning is essential to extend these services. The existing programs within the primary healthcare system, which already cater to men through initiatives like the middle-aged program or pre-pregnancy care program for women, serve as a suitable platform to address this crucial aspect of family health. Gynecologists, midwives, and other primary healthcare providers can play a pivotal role in encouraging men to seek preconception care. A significant factor in this process may be the insufficient awareness among healthcare providers themselves. In alignment with Iran’s population policies aimed at safeguarding the population, prioritizing the involvement of men is crucial. Given the research limitations, it is recommended that future studies focus on a population consisting solely of couples intending to conceive within the next six months
Conclusion
A significant number of men have tried to conceive while having at least one risk factor affecting the health of conception or the health of the fetus/newborn.
Acknowledgments: This article is derived from the midwifery master’s thesis of Somayeh Mashayekhi, registered at Ahvaz Jundishapur University of Medical Sciences. The authors express gratitude to the pregnant women who took part in the study, as well as to Ahvaz Jundishapur University of Medical Sciences for providing financial support for the research.
Conflicts of Interests: The authors declared no conflicts of interests.
Ethical Permissions: The study received approval from the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1397.352). To adhere to ethical standards, informed consent was acquired following a detailed explanation of the research objectives to the participants. Furthermore, the results were disclosed in accordance with confidentiality principles, ensuring anonymity by refraining from mentioning any names.
Authors’ Contribution: Mashayekhi S (First Author), Introduction Writer/Main Researcher/Discussion Writer (30%); Abbaspoor Z (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (15%); Cheraghian B (Third Author), Discussion Writer/Statistical Analyst (15%); Javadnoori M Introduction Writer/Methodologist/Main Researcher/Discussion Writer (40%)
Funding/Support: This study was supported by the Jundishapur University of Medical Sciences (Grant No.: RHPRC-9705).
Keywords:
References
1. Almeling R, Waggoner MR. More and less than equal: How men factor in the reproductive equation. Gend Soc. 2013;27(6):821-42. [Link] [DOI:10.1177/0891243213484510]
2. Mumford SL, Michels KA, Salaria N, Valanzasca P, Belizán JM. Preconception care: It's never too early. Reprod Health. 2014;11:73. [Link] [DOI:10.1186/1742-4755-11-73]
3. Jack BW, Atrash H, Coonrod DV, Moos M-K, O'donnell J, Johnson K. The clinical content of preconception care: An overview and preparation of this supplement. Am J Obstet Gynecol. 2008;199(6 Suppl B):S266-79. [Link] [DOI:10.1016/j.ajog.2008.07.067]
4. Dunlop AL, Jack B, Frey K. National recommendations for preconception care: The essential role of the family physician. J Am Board Fam Med. 2007;20(1):81-4. [Link] [DOI:10.3122/jabfm.2007.01.060143]
5. Johnson K, Posner SF, Biermann J, Cordero JF, Atrash HK, Parker CS, et al. Recommendations to improve preconception health and health care-United States: Report of the CDC/ATSDR preconception care work group and the select panel on preconception care. MMWR Recomm Rep. 2006;55(RR-6):1-23. [Link] [DOI:10.1037/e506902006-001]
6. Casey FE, Sonenstein FL, Astone NM, Pleck JH, Dariotis JK, Marcell AV. Family planning and preconception health among men in their mid-30s: Developing indicators and describing need. Am J Mens Health. 2016;10(1):59-67. [Link] [DOI:10.1177/1557988314556670]
7. O'Brien AP, Hurley J, Linsley P, McNeil KA, Fletcher R, Aitken JR. Men's preconception health: A primary health-care viewpoint. Am J Mens Health. 2018;12(5):1575-81. [Link] [DOI:10.1177/1557988318776513]
8. Choiriyyah I, Sonenstein FL, Astone NM, Pleck JH, Dariotis JK, Marcell AV. Men aged 15-44 in need of preconception care. Matern Child Health J. 2015;19(11):2358-65. [Link] [DOI:10.1007/s10995-015-1753-7]
9. Frey KA, Engle R, Noble B. Preconception healthcare: What do men know and believe?. J Mens Health. 2012;9(1):25-35. [Link] [DOI:10.1016/j.jomh.2011.11.001]
10. Wright C, Milne S, Leeson H. Sperm DNA damage caused by oxidative stress: Modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod Biomed Online. 2014;28(6):684-703. [Link] [DOI:10.1016/j.rbmo.2014.02.004]
11. Rabiei Z, Shariati M, Mogharabian N, Tahmasebi R, Ghiasi A, Motaghi Z. Men's knowledge of preconception health: A systematic review. J Family Med Prim Care. 2023;12(2):201-7. [Link] [DOI:10.4103/jfmpc.jfmpc_1090_22]
12. Gage JD, Kirk R. First-time fathers: Perceptions of preparedness for fatherhood. Can J Nurs Res. 2002;34(4):15-24. [Link]
13. Van Der Zee B, De Wert G, Steegers EA, De Beaufort ID. Ethical aspects of paternal preconception lifestyle modification. Am J Obstet Gynecol. 2013;209(1):11-6. [Link] [DOI:10.1016/j.ajog.2013.01.009]
14. Mitchell EW, Levis DM, Prue CE. Preconception health: Awareness, planning, and communication among a sample of US men and women. Matern Child Health J. 2012;16(1):31-9. [Link] [DOI:10.1007/s10995-010-0663-y]
15. Czeizel AE, Czeizel B, Vereczkey A. The participation of prospective fathers in preconception care. Clin Med Insights Reprod Health. 2013;7:1-9. [Link] [DOI:10.4137/CMRH.S10930]
16. Mortazavi F, Delara M, Akaberi A. Male involvement in prenatal care: Impacts on pregnancy and birth outcomes. Nurs Midwifery J. 2014;12(1):63-71. [Persian] [Link]
17. Motlagh ME, Torkestani F, Ashrafian Amiri H, Rabiee SM, Radpooyan L, Nasrollahpour Shirvani SD, et al. Iranian husbands' involvement in prenatal care, childbirth and postpartum: Viewpoints of the mothers. J Babol Univ Med Sci. 2017;19(5):29-37. [Persian] [Link]
18. Goldberg D, Williams P. A user's guide to the general health questionnaire. London: Nfer-Nelson; 1991. [Link]
19. Nazifi M, Mokarami H, Akbaritabar A, Faraji Kujerdi M, Tabrizi R, Rahi A. Reliability, validity and factor structure of the Persian translation of general health questionnaire (GHQ-28) in hospitals of Kerman university of medical sciences. J Adv Biomed Sci. 2013;3(4):336-42. [Persian] [Link] [DOI:10.17795/jhealthscope-15547]
20. Taghavi SMR. Validity and reliability of the general health questionnaire (GHQ-28) in college students of Shiraz University. J Psychol. 2002;5(4):381-98. [Persian] [Link]
21. Fang Y, Wang Y, Peng M, Xu J, Fan Z, Liu C, et al. Effect of paternal age on offspring birth defects: A systematic review and meta-analysis. Aging. 2020;12(24):25373-94. [Link] [DOI:10.18632/aging.104141]
22. Wiener-Megnazi Z, Auslender R, Dirnfeld M. Advanced paternal age and reproductive outcome. Asian J Androl. 2012;14(1):69-76. [Link] [DOI:10.1038/aja.2011.69]
23. Ayatollahi SMT, Ghoreshizadeh Z. Prevalence of obesity and overweight among adults in Iran. Obes Rev. 2010;11(5):335-7. [Link] [DOI:10.1111/j.1467-789X.2010.00725.x]
24. Agricola E, Gesualdo F, Carloni E, D'Ambrosio A, Russo L, Campagna I, et al. Investigating paternal preconception risk factors for adverse pregnancy outcomes in a population of internet users. Reprod Health. 2016;13:37. [Link] [DOI:10.1186/s12978-016-0156-6]
25. Pauli EM, Legro RS, Demers LM, Kunselman AR, Dodson WC, Lee PA. Diminished paternity and gonadal function with increasing obesity in men. Fertil Steril. 2008;90(2):346-51. [Link] [DOI:10.1016/j.fertnstert.2007.06.046]
26. Rybar R, Kopecka V, Prinosilova P, Markova P, Rubes J. Male obesity and age in relationship to semen parameters and sperm chromatin integrity. Andrologia. 2011;43(4):286-91. [Link] [DOI:10.1111/j.1439-0272.2010.01057.x]
27. Sallmén M, Sandler DP, Hoppin JA, Blair A, Baird DD. Reduced fertility among overweight and obese men. Epidemiology. 2006;17(5):520-3. [Link] [DOI:10.1097/01.ede.0000229953.76862.e5]
28. Stokes VJ, Anderson RA, George JT. How does obesity affect fertility in men-and what are the treatment options?. Clin Endocrinol. 2015;82(5):633-8. [Link] [DOI:10.1111/cen.12591]
29. Hammoud AO, Wilde N, Gibson M, Parks A, Carrell DT, Meikle AW. Male obesity and alteration in sperm parameters. Fertil Steril. 2008;90(6):2222-5. [Link] [DOI:10.1016/j.fertnstert.2007.10.011]
30. Garfield CF, Duncan G, Rutsohn J, McDade TW, Adam EK, Coley RL, et al. A longitudinal study of paternal mental health during transition to fatherhood as young adults. Pediatrics. 2014;133(5):836-43. [Link] [DOI:10.1542/peds.2013-3262]
31. Crijns I, Bos J, Knol M, Straus S, De Jong-Van Den Berg L. Paternal drug use: Before and during pregnancy. Expert Opin Drug Saf. 2012;11(4):513-8. [Link] [DOI:10.1517/14740338.2012.674109]
32. De Santis M, Cesari E, Cavaliere A, Ligato MS, Nobili E, Visconti D, et al. Paternal exposure and counselling: Experience of a teratology information service. Reprod Toxicol. 2008;26(1):42-6. [Link] [DOI:10.1016/j.reprotox.2008.06.003]
33. Engeland A, Bjørge T, Daltveit AK, Skurtveit S, Vangen S, Vollset SE, et al. Effects of preconceptional paternal drug exposure on birth outcomes: Cohort study of 340000 pregnancies using Norwegian population‐based databases. Br J Clin Pharmacol. 2013;75(4):1134-41. [Link] [DOI:10.1111/j.1365-2125.2012.04426.x]
34. Van Rooij IA, Wijers CH, Rieu PN, Hendriks HS, Brouwers MM, Knoers NV, et al. Maternal and paternal risk factors for anorectal malformations: A Dutch case‐control study. Birth Defects Res Part A Clin Mol Teratol. 2010;88(3):152-8. [Link] [DOI:10.1002/bdra.20649]
35. Bailey JA, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Men's and women's patterns of substance use around pregnancy. Birth. 2008;35(1):50-9. [Link] [DOI:10.1111/j.1523-536X.2007.00211.x]
36. Lassi ZS, Imam AM, Dean SV, Bhutta ZA. Preconception care: Caffeine, smoking, alcohol, drugs and other environmental chemical/radiation exposure. Reprod Health. 2014;11(3):S6. [Link] [DOI:10.1186/1742-4755-11-S3-S6]
37. Robledo CA, Yeung E, Mendola P, Sundaram R, Maisog J, Sweeney AM, et al. Preconception maternal and paternal exposure to persistent organic pollutants and birth size: The LIFE study. Environ Health Perspect. 2015;123(1):88-94. [Link] [DOI:10.1289/ehp.1308016]
38. Abdoli S, Masoumi SZ, Kazemi F. Environmental and occupational factors and higher risk of couple infertility: A systematic review study. Middle East Fertil Soc J. 2022;27:33. [Link] [DOI:10.1186/s43043-022-00124-4]
39. Babakhah L, Azad L, Arbabian M, Tavalaee M, Bahadorani M, Nasr Esfahani MH. Influence of occupational exposures on sperm parameters and chromatin structure. Cell Tissue J. 2017;8(1):52-68. [Persian] [Link]
40. Javadnoori M, Hajizadeh M, Javadifar N, Hossein Haghighizadeh M. Sexual and reproductive healthcare needs of Iranian men: A cross-sectional study. Int J Reprod Biomed. 2018;16(12):ijrm.v16i12.3681. [Link] [DOI:10.18502/ijrm.v16i12.3681]
41. Frey KA, Navarro SM, Kotelchuck M, Lu MC. The clinical content of preconception care: Preconception care for men. Am J Obstet Gynecol. 2008;199(6):S389-95. [Link] [DOI:10.1016/j.ajog.2008.10.024]
42. Goodfellow A, Frank J, McAteer J, Rankin J. Improving preconception health and care: A situation analysis. BMC Health Serv Res. 2017;17(1):595. [Link] [DOI:10.1186/s12913-017-2544-1]